Vasectomy
What is a Vasectomy?
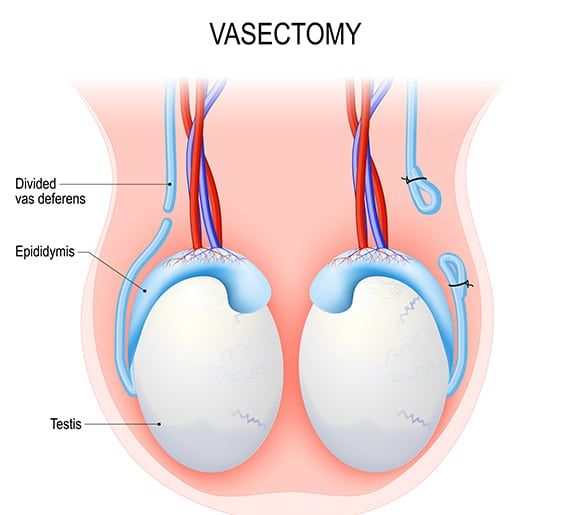
A vasectomy is a surgical procedure in which the vas deferens, the tubes that carry sperm from the testicles to the urethra, are cut or blocked. This prevents sperm from being present in the semen and, thus, prevents pregnancy. It is a permanent form of birth control for men.
Although vasectomy is considered a permanent form of birth control, there are some methods to reverse it, such as Vasectomy reversal surgery, but it is not guaranteed.
Who is Suitable for Vasectomy?
Vasectomy is typically recommended for men who are sure they do not want any more children or want a permanent birth control form. It is considered a safe and effective method of birth control for men.
However, there are certain factors that a healthcare provider will consider before recommending a vasectomy, such as:
- Age: Men older and have completed their families are more likely to be suitable candidates for vasectomy.
- Health: Men with certain medical conditions that may increase the risk of complications from the procedure may not be suitable candidates.
- Lifestyle: Men in a stable, long-term relationship who have discussed the decision with their partner are more likely to be suitable candidates.
It's essential to have a thorough discussion with your doctor about your individual circumstances before deciding on a vasectomy.
What are the Benefits of Vasectomy?
Vasectomy has several benefits, including:
- High effectiveness: Vasectomy is considered one of the most effective forms of birth control available for men, with a failure rate of less than 1%.
- Permanent: Unlike other forms of birth control, vasectomy is permanent and does not require ongoing maintenance.
- Low complication rate: Vasectomy is a relatively simple procedure with a low complication rate.
- No effect on sexual function: Vasectomy does not affect a man's ability to have an erection, ejaculate or have an orgasm, and there are no changes in sexual sensation.
- Safe: Vasectomy is a safe procedure with a very low risk of serious complications.
- Cost-effective: Vasectomy is a one-time cost and is less expensive over time than other forms of birth control.
How Common Are Vasectomies?
Vasectomy has been used for about a century as a means of sterilisation. It has a long track record as a safe and effective method of contraception and is relied upon by millions of people worldwide.
Roughly 5 per cent of all married couples of reproductive age have Vasectomies.
About 15 per cent of couples rely on female sterilisation for birth control.
The prevalence of men undergoing the procedure increases with higher education and income levels.
Vasectomy vs Female Sterilisation?
Regardless of how it is performed, vasectomy offers many advantages as a method of birth control. It is a highly effective one-time procedure that provides permanent contraception like female sterilisation.
Vasectomy, however, is much simpler than female sterilisation, has a lower incidence of complications, and is much less expensive.
Types of Vasectomy
Vasectomy can be performed by various surgical techniques, including:
Conventional Vasectomy
The testicles and scrotum are cleaned with an antiseptic solution.
- After thoroughly evaluating and discussing the potential side effects and complications, Dr Wang usually performs a vasectomy under general anaesthesia.
- Two small punctures or holes are made on the scrotum,
- A part of the vas deferens is removed through the opening.
- The cut ends of the vas deferens are then tied off with a stitch.
- In some cases, electrocautery is typically used to seal the ends with heat.
- The skin is closed with absorbable sutures.
The procedure takes 20 to 30 minutes.
No-Scalpel Technique
It is a technique that uses a small clamp rather than a scalpel to puncture the scrotum.
The clamp is poked through the skin of the scrotum and then opened. This technique reduces bleeding, infection and pain and no skin stitches are often needed.
Recovery After a Vasectomy
After a vasectomy, the patient will probably feel sore for a few days and should rest for at least one day. However, he can expect to recover completely in less than a week.
Many men have the procedure on a Friday and return to work on Monday.
Post Vasectomy Care
Dr Wang will go through all the precautionary measures during the initial consultation and provide a patient information sheet.
After vasectomy, it usually takes a few months for all remaining sperm to ejaculate or reabsorb. Instructions to follow after surgery may include the following:
- Avoid heavy lifting for a week
- Apply cold packs to the area
- Wearing snug underwear to support the scrotum
- Get plenty of rest
How Soon Can You Have Sex After a Vasectomy?
A man can resume sexual activity within a few days after vasectomy, but precautions should be taken against pregnancy until a test shows that his semen is free of sperm.
Alternative birth control methods must be used until a semen sample test shows a zero sperm count. Generally, this test is performed at the 3 month mark and after the patient has had more than 20 post-vasectomy ejaculations. If sperm are still present in the semen, the patient is told to return later for a repeat test.
A rare postoperative side effect of vasectomy is epididymitis/orchitis (defined as painful, swollen, and tender epididymis or testis). This condition can be treated with heat and usually clears within a week.
Risks with Vasectomy
Although complications such as swelling, bruising, inflammation, and infection may occur, they are relatively uncommon and rarely severe.
Nevertheless, men who develop these symptoms should inform their physician.
The most common risks include the following:
- Infection: There is a small risk of infection at the incision site. This can usually be treated with antibiotics.
- Bleeding: There is a small risk of bleeding at the incision site. This can usually be treated with a minor surgical procedure.
- Sperm granuloma: A small lump may form at the site of the cut vas deferens. This is called sperm granuloma, which is typically painless and does not require treatment, but in some cases, it may cause discomfort.
- Chronic pain: In rare cases, men may experience chronic pain, called post-vasectomy pain syndrome, which can usually be managed with pain medication.
- Recanalisation: In rare cases, the vas deferens can grow back together, resulting in the return of fertility, which is known as recanalisation.
- Failure: Even though vasectomy is considered a highly effective form of birth control, there is still a slight chance of failure. The failure rate is less than 1%, but using another form of birth control is essential until a semen analysis confirms that there is no sperm present.
What if Vasectomy is Delayed?
If a vasectomy is delayed, it does not typically cause any long-term health problems. However, it may increase the risk of unintended pregnancy. Using another form of birth control is essential until a semen analysis confirms that there is no sperm present.
Vasectomy FAQs
What are the disadvantages of vasectomy?
The chief advantage of vasectomy is its permanence. The procedure is simple, but reversing it is difficult, expensive, and often unsuccessful.
How about storing semen in a sperm bank?
It is possible to store semen in a sperm bank to preserve the possibility of producing a pregnancy at some future date. However, this can be costly, and the sperm in stored semen do not always remain able to cause pregnancy.
When should the decision about vasectomy be made?
Doctors advise that vasectomy be undertaken only by men who are prepared to accept that they will no longer be able to father a child. The decision should be considered along with other contraceptive options and discussed with a professional counsellor.
Men who are married or in a serious relationship should also discuss the issue with their partners.
Does vasectomy protect against HIV and other STDs?
Although the procedure is highly effective in preventing pregnancy, vasectomy does not offer any protection whatsoever against HIV/AIDS or any other sexually transmitted diseases (STDs).
Consequently, vasectomised men must continue to use condoms, preferably latex, which offers considerable protection against the spread of disease in any sexual encounter that carries the risk of contracting or transmitting infection.
How does vasectomy affect masculinity and sexuality?
Not at all.
Vasectomy does not affect the production or release of testosterone, the male hormone responsible for a man’s sex drive, beard, deep voice, and other masculine traits. The operation also does not affect sexuality.
Erections, climaxes, and the amount of ejaculation remain the same. Occasionally, a man may experience sexual difficulties after vasectomy, but these almost always have an emotional basis and can usually be alleviated with counselling.
More often, men who have undergone the procedure, and their partners, find that sex is more spontaneous and enjoyable once they are freed from concerns about contraception and accidental pregnancy.
Are there immune reactions to sperm after vasectomy?
After vasectomy, the testes continue to make sperm. When the sperm cells die, they are absorbed by the body, much like unused sperm in a non-vasectomized man.
Nevertheless, many vasectomised men develop immune reactions to sperm, although current evidence indicates that these reactions do not cause any harm.
Ordinarily, sperm does not come in contact with immune cells, so they do not elicit an immune response. But vasectomy breaches the barriers that separate immune cells from sperm, and many men develop anti-sperm antibodies after the procedure.
Immune reactions against parts of one’s own body sometimes cause disease. (Rheumatoid arthritis, juvenile diabetes, and multiple sclerosis are some of the illnesses suspected or known to be caused by immune reactions of this type, as well as possibly contributing to the development of atherosclerosis).
Researchers have found no evidence that vasectomised men were more likely than others to develop heart disease or any other immune illnesses.
Is there an increased risk of prostate cancer after vasectomy?
Many studies show no increase in cancer among vasectomised men, even though three hospital-based studies published in 1990 reported a positive correlation between vasectomy and prostate cancer.
This was evaluated by the WHO, as well as possible associations between vasectomy and testicular cancer. The assembled experts concluded that a causal relationship between vasectomy and prostate cancer or testis was unlikely. Additional studies of vasectomised men have reinforced this.
Vasectomy Reversal Surgery
What is Vasectomy Reversal?
Vasectomy reversal is a surgical procedure in which the vas deferens, the tubes that were cut or blocked during a vasectomy, are reconnected. This allows sperm to enter once again the semen, which can potentially restore fertility.
Types of Vasectomy Reversal
There are two main types of vasectomy reversal:
- Vasovasostomy: This procedure reconnects the ends of the cut vas deferens. This is the most common type of vasectomy reversal and has the highest success rate.
- Vasoepididymostomy: This procedure connects the vas deferens to the epididymis, a small organ located next to the testicles. This procedure is typically used when there is a blockage in the epididymis and is less successful than vasovasostomy.
Success Rate of Vasectomy Reversal
Vasectomy reversal is possible, but it is a complex procedure typically less successful than the original vasectomy. The success rate of a vasectomy reversal depends on several factors, such as:
- The time since the original vasectomy: The longer the time since the original vasectomy, the lower the success rate.
- The type of vasectomy reversal: Vasovasostomy has a higher success rate than vasoepididymostomy.
- The age and fertility of the partner: The younger the partner and the better their fertility, the higher the chances of pregnancy.
Vasectomy Reversal Risks
Vasectomy reversal is considered safe, but like any surgical procedure, it carries certain risks, such as bleeding, infection, pain, and discomfort. Additionally, there is a risk of failure to restore fertility and injury to surrounding structures.
Reversing a vasectomy does not guarantee a return to fertility. It is considered a permanent form of birth control, so it should be thought through carefully and be sure of the decision before the procedure.