Enlarged Prostate
What is an Enlarged Prostate?
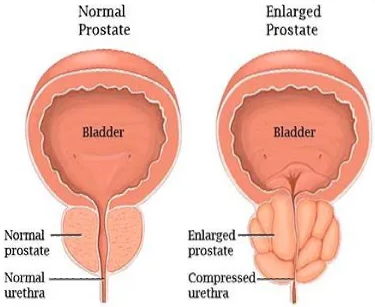
Enlarged prostate is also known as Benign Prostatic Hyperplasia (BPH). Benign Prostatic Hyperplasia, or BPH, is a condition in which the prostate gland, a small gland located below the bladder in men, becomes enlarged. This can cause symptoms such as difficulty urinating, frequent urination, and a weak urine stream.
BPH is a common condition in older men and is not cancerous. Treatment options may include medication, lifestyle changes, or surgery.
How Does BPH Impact Your Anatomy and Health?
BPH can impact your anatomy and health in several ways:
- Urinary symptoms: As the prostate enlarges, it can put pressure on the urethra (the tube that carries urine out of the body), making urination more difficult. This can cause symptoms such as difficulty starting urination, a weak urine stream, and frequent urination.
- Urinary tract infections: As the prostate enlarges, it can also increase the risk of urinary tract infections (UTIs) due to the difficulty in completely emptying the bladder.
- Bladder damage: If BPH is left untreated, it can lead to bladder damage. The bladder may be forced to work harder to push urine out, causing it to become thicker and weaker over time.
- Kidney damage: In rare cases, BPH can cause damage to the kidneys if the urine flow is blocked for a long time.
- Stone formation: poor drainage of bladder and residual urine can lead to stones forming in the bladder.
Who is at Risk for BPH?
Enlarged prostate, or BPH, is a common condition that affects many older men. Risk factors include:
- Age: The risk of BPH increases as men age. Most men will have some degree of prostate enlargement by age 80.
- Family history: Men with a family history of BPH are more likely to develop the condition themselves.
- Race: BPH is more common in men of African descent.
- Hormones: The prostate gland is influenced by male hormones, particularly dihydrotestosterone (DHT). Men with higher levels of DHT may be at increased risk of BPH.
- Lifestyle factors: Some studies suggest that a diet high in fat and meat and low in fruits and vegetables may increase the risk of BPH.
Causes of Benign Prostatic Hyperplasia
BPH is a benign enlargement of the prostate gland. It occurs due to proliferation and increased growth (hyperplasia) of the epithelial and stromal layers of the prostate gland.
The exact cause of BPH is not known. However, several factors play a role in its development.
- Hormones: The prostate gland is influenced by male hormones, particularly dihydrotestosterone (DHT). As men age, the levels of DHT in the prostate may increase, leading to prostate cell growth and an enlarged prostate.
- Genetics: There is a genetic component to BPH, as men with a family history of the condition are more likely to develop it themselves.
- Inflammation: Some studies suggest that chronic prostate inflammation may contribute to the development of BPH.
- Lifestyle Factors: Certain lifestyle factors like diet, obesity and lack of physical activity may also play a role in developing BPH.
These factors are not necessarily causes of BPH but rather potential contributing factors. There is no definitive way to prevent BPH, but maintaining a healthy lifestyle, eating a balanced diet, and regularly monitoring your prostate health with your doctor can help.
Symptoms of Benign Prostatic Hyperplasia
The prostate gland is situated below the urinary bladder in men and surrounds the proximal urethra. Enlarged prostate glands cause symptoms as a result of the constriction of the urethra, which results in:
- Difficulty starting urination
- Weak or interrupted urine stream
- Frequent urination, including at night
- Incomplete emptying of the bladder
- Straining to urinate
- Urinary tract infections
Stages Of Benign Prostatic Hyperplasia
BPH is typically classified into four stages based on the size of the prostate and the severity of symptoms. These stages are:
- Stage 1: The prostate is slightly enlarged, and symptoms are mild.
- Stage 2: The prostate is moderately enlarged, and symptoms are moderate.
- Stage 3: The prostate is significantly enlarged, and symptoms are severe.
- Stage 4: The prostate is significantly enlarged, and severe symptoms and urinary retention (inability to empty the bladder) may occur.
Your surgeon can determine the growth of a benign tumour, and its size can determine the severity of the symptoms. However, prostate size is not always an indicator of symptom severity.
How is Benign Prostatic Hyperplasia Diagnosed?
BPH is typically diagnosed through a physical exam, a medical history, and diagnostic tests.
- Medical History: The doctor will take a detailed medical history, including any symptoms you may be experiencing and any other health conditions you have. They will also ask about any medications you take, including over-the-counter medicines and supplements.
- Physical Exam: During a physical exam, the doctor will feel the prostate gland through the rectum (digital rectal exam) to check for any lumps or irregularities. They may also check for any other signs of prostate problems, such as an enlarged prostate.
- Diagnostic Tests: The doctor may order one or more diagnostic tests to confirm the BPH diagnosis and rule out other conditions. These tests may include the following:
- Prostate-specific antigen (PSA) blood test
- Urinalysis
- Urodynamic Tests are used to measure the function of the urinary tract. They can be used to evaluate how well the bladder and urethra are working and measure the pressure in the bladder.
- Imaging tests such as ultrasound, MRI and CT scans can be used to get a detailed view of the prostate and the surrounding structures.
How is Benign Prostatic Hyperplasia Treated?
BPH can be treated in several ways, depending on the severity of the condition and the symptoms experienced. Treatment options include:
- Lifestyle changes: Making specific changes can also help alleviate BPH symptoms. Drinking less fluid in the evening, avoiding caffeine and alcohol, and avoiding activities that cause stress to the bladder, such as cycling, can be beneficial.
- Watchful Waiting: If symptoms are mild and not affecting the quality of life, some men may wait and monitor the condition rather than undergo treatment.
- Medications: Several types of drugs can help relieve symptoms of BPH.
- Surgery: If symptoms are severe or medication is not working, surgery may be recommended.
Not all men with BPH will require treatment, and the appropriate treatment will depend on the individual case. Your doctor will advise you on the best treatment option based on your specific symptoms and medical history. Regular check-ups with your doctor will help to monitor any changes in your prostate health.
Medications for BPH Treatment
Some medicines work best in cases with mild to moderate symptoms and include
- Alpha-blockers – They relax the neck of the bladder and surrounding tissues, making urination easier.
- 5 Alpha-Reductase Inhibitors – This group of drugs results in size reduction of the prostate gland, again making urination easier
- Combination – In some instances, a combination approach can also be given; these work by relaxing bladder muscles and shrinking the prostate gland.
- PDE5 inhibitors – They are practical, presumably due to the relaxation of the smooth muscle fibres of the bladder and prostate, especially useful in men with erectile dysfunction
- Anticholinergics or beta3 agonists (Mirabegron) – They are not the first line for BPH. However, they relieve overactive bladder symptoms and are helpful adjuncts, especially for men suffering severe urge or urge incontinence.
Advanced BPH Treatments
- Urolift - involves sutures placed into the prostate that effectively squeezes the urethra open.
- Transurethral Resection Of The Prostate – TURP. A telescope is inserted via the urethra, and the enraged part of the prostate gland is removed.
- Transurethral Incision Of The Prostate – TUIP (or Bladder Neck Incision BNI) - for this procedure, incisions are only made in the prostate gland to make urination easier
- Rezum – Using water vapour (steam) injected into the prostate causes the enlarged parts of the prostate to die and be reabsorbed by the body.
- Laser Therapy - where amplified light energy generates heat to destroy prostatic tissue. There are many different types of laser therapy for BPH.
- Robot-Assisted Prostatectomy - uses a robotic approach to remove the enlarged part of the prostate gland.
- Open Prostatectomy – open approach via the perineal or public to access and remove the enlarged part of the prostate gland.
- Embolisation – where the blood supply to the prostate is cut, shrinkage in size is expected to allow easier passing of urine.
What if Benign Prostatic Hyperplasia is Untreated?
If left untreated, the symptoms caused by BPH may continue to cause the patient mild or severe distress, depending upon the growth of the prostate gland.
Further distress can result from frequent worrying about urinating and constant visits to the bathroom when at work or attending events and at night.
Sometimes, complications such as frequent urine infections, an inability to pass urine (retention), bladder stone formation, and kidney damage can occur.
Prostatitis
What is Prostatitis?
Prostatitis is when the prostate gland, a small gland located below the bladder in men, becomes inflamed. There are several types of prostatitis, including acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis.
Symptoms of prostatitis can include pain or discomfort in the pelvic area, difficulty urinating, frequent urination, and pain or discomfort during ejaculation.
Causes of Prostatitis
The causes of prostatitis can vary depending on the type, but several factors are thought to play a role in its development.
- Bacterial infection: Acute bacterial prostatitis, the most common type of prostatitis, is caused by a bacterial infection of the prostate gland. The bacteria can enter the prostate through the urethra or the bloodstream.
- Chronic bacterial prostatitis: This type of prostatitis is also caused by a bacterial infection, but the symptoms can be more persistent and long-lasting.
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): The cause of this type of prostatitis is not fully understood, but it is thought to be related to chronic inflammation of the prostate gland.
- Asymptomatic inflammatory prostatitis: This type of prostatitis does not cause symptoms, but inflammation can be detected during routine check-ups or tests for other conditions.
- Risk factors such as a history of urinary tract infections, previous prostate surgery, and a sedentary lifestyle may also increase the risk of developing prostatitis.
Treatment for Prostatitis
Treatment for prostatitis, an inflammation of the prostate gland, will depend on the type of prostatitis and the underlying cause.
- Acute bacterial prostatitis: This type of prostatitis is caused by a bacterial infection and is treated with antibiotics. The course of antibiotics is usually 4-6 weeks.
- Chronic bacterial prostatitis: This type of prostatitis is also caused by a bacterial infection, but the symptoms can be more persistent and long-lasting. Treatment is similar to acute bacterial prostatitis and includes a longer course of antibiotics, up to 12 weeks.
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): The cause of this type of prostatitis is not fully understood, and treatment can be more complex. It usually includes a combination of different therapies such as antibiotics, alpha-blockers, anti-inflammatory medication, physical therapy, and dietary and lifestyle changes.
- Asymptomatic inflammatory prostatitis: This type of prostatitis does not cause symptoms, but inflammation can be detected during routine check-ups or tests for other conditions. Treatment is usually unnecessary, but antibiotics are prescribed if there is an underlying infection.
- Pain management is also an essential aspect of treatment; it may include non-steroidal anti-inflammatory drugs (NSAIDs) and other medications, such as tricyclic antidepressants, which can help reduce pain and improve sleep.