Other Cancers
Testicular Cancer
What is Testicular Cancer?
Testicular cancer is a type of cancer that develops in the testicles, which are located in the scrotum. It occurs when abnormal cells in the testicles divide and grow uncontrollably. Testicular cancer most commonly affects men between the ages of 15 and 35, but it can occur at any age.
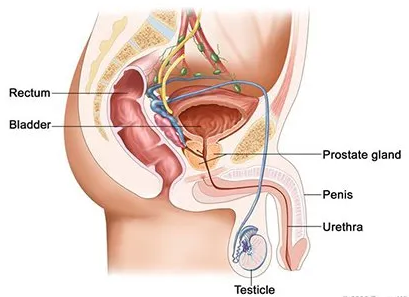
How Does Testicular Cancer Impact Your Anatomy and Health?
Testicular cancer can impact a man's anatomy by spreading to nearby lymph nodes and organs, such as the lungs or brain. If cancer has spread beyond the testicles, it can also affect a man's overall health and quality of life.
Types of Testicular Cancer
There are two main types of testicular cancer: Seminoma and Non-Seminoma.
Seminoma: This type of testicular cancer develops from cells called germ cells responsible for producing sperm. Seminoma grows and spreads slowly and is usually more responsive to treatment.
Non-Seminoma: This type of testicular cancer develops from cells called embryonal cells and yolk sac cells. Non-Seminoma tends to grow and spread more quickly than seminoma and is less responsive to treatment.
Non-Seminoma subtypes include
- Embryonal Carcinoma: The most common subtype of non-seminoma.
- Yolk Sac Carcinoma: This testicular cancer is rare and usually found in younger men.
- Choriocarcinoma: This type of cancer is extremely rare and often fast-growing.
- Teratoma: This type of cancer is rare and can be benign or malignant.
Some testicular cancers can have features of both seminoma and non-seminoma, called mixed germ cell tumours, which can be treated differently.
How Common is Testicular Cancer?
Although testicular cancer is rare, it is one of the most common cancers in men aged between 15 and 45. It is also one of the most curable cancers if found early.
Testicular Cancer Causes and Risk Factors
The exact causes of testicular cancer are not fully understood, but certain factors may contribute to its development. These include
- Age: Testicular cancer is most common in men between the ages of 15 and 35.
- Abnormal development of the testicles: Men who had undescended testicles at birth may have a higher risk of developing testicular cancer.
- Genetic mutations: Certain genetic mutations may increase the risk of testicular cancer.
- Family history: Men with a family history of testicular cancer are at a higher risk of developing the disease.
- Race and Ethnicity: White men have a higher incidence of testicular cancer than men of other races.
- HIV infection: HIV-positive men have a higher risk of testicular cancer.
Symptoms of Testicular Cancer
Symptoms of testicular cancer may include:
- A lump or swelling in the testicle is usually painless.
- A feeling of heaviness in the scrotum.
- A dull ache in the lower abdomen or scrotum.
- A sudden collection of fluid in the scrotum.
- Pain or discomfort in the testicles or scrotum.
- Enlargement of breast tissue (gynecomastia)
- Back pain
- Changes in how the testicles feel to the touch.
Many men with testicular cancer do not experience symptoms in the early stages of the disease. This is why it is essential for all men to be aware of the symptoms of testicular cancer and to seek medical attention if they notice any changes in their testicles or scrotum.
Diagnosis of Testicular Cancer
Testicular cancer is usually diagnosed through a combination of physical examination, imaging tests, and biopsy. The diagnostic process may include
- Physical examination,
- Ultrasound,
- Biopsy,
- Blood test: can be done to measure the level of tumour markers such as alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-hCG), and lactate dehydrogenase (LDH). Elevated levels of these markers may indicate the presence of testicular cancer.
- Additional tests: Additional tests may be needed to determine the cancer stage, such as computed tomography (CT) scan, magnetic resonance imaging (MRI), or chest X-ray.
Testicular cancer can be tricky to diagnose, especially in the early stages. If you have any symptoms or concerns, you should see a doctor as soon as possible.
Treatment for Testicular Cancer
Treatment for testicular cancer depends on the cancer stage, the type of cancer, and the patient's overall health. The main treatments for testicular cancer include
- Surgery: Surgery to remove the affected testicle (radical inguinal orchiectomy) is the primary treatment for testicular cancer.
- Radiation Therapy: Radiation therapy uses high-energy radiation to kill cancer cells. It is usually used as an adjuvant therapy (additional treatment) after surgery for seminoma-type cancer or as a primary treatment for a non-seminoma type of cancer.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It is usually used as an immediate treatment for advanced stages of testicular cancer or the recurrence of the disease after surgery.
- Retroperitoneal Lymph Node Dissection (RPLND): This surgical procedure removes lymph nodes from the back of the abdomen. It is usually done for non-seminoma types of cancer or recurrence of the disease after surgery.
- Monitoring: Regular follow-up examinations and imaging tests are essential to detect any recurrence as soon as possible.
Testicular cancer is highly curable, especially when it is detected and treated early. With appropriate treatment, most men with testicular cancer will be cured.
What if Testicular Cancer is Untreated?
If testicular cancer is not treated, it can cause serious health complications and affect the quality of life. Symptoms of advanced testicular cancer may include back pain, shortness of breath, and neurological symptoms such as headaches or seizures.
Seek prompt medical attention if you suspect you may have testicular cancer, even if the symptoms are mild or not present. Early detection and treatment of testicular cancer can significantly improve the chances of recovery.
Testicular cancer can recur, even after treatment, especially in advanced stages. Regular follow-up examinations and imaging tests are essential to detect any recurrence as soon as possible.
Penile Cancer
What is Penile Cancer?
Penile cancer is a rare type of cancer that affects the skin and tissues of the penis. It occurs when abnormal cells in the penis divide and grow uncontrollably.
Anatomy of the Penis
The penis is a rod-shaped male reproductive organ that passes sperm and urine from the body. It contains two types of erectile tissue (spongy tissue with blood vessels that fill with blood to make an erection):
- Corpora Cavernosa: The two columns of erectile tissue that form most of the penis.
- Corpus Spongiosum: The single column of erectile tissue forms a small portion of the penis. The corpus spongiosum surrounds the urethra (the tube through which urine and sperm pass from the body).
The erectile tissue is wrapped in connective tissue and covered with skin. The glans (head of the penis) are covered with loose skin called the foreskin.
What are the Types of Penile Cancer?
There are several types of penile cancer, including
- Squamous cell carcinoma: This is the most common type of penile cancer, and it begins in the flat, thin cells that line the surface of the penis.
- Basal cell carcinoma: This type of penile cancer is rare and begins in the cells at the base of the epidermis.
- Melanoma: This type of penile cancer is rare and begins in the skin's pigment-producing cells.
Causes and Risk Factors for Penile Cancer
Risk factors for penile cancer include the following:
- Being age 60 or older,
- Having phimosis (a condition in which the foreskin of the penis cannot be pulled back over the glans) and chronic inflammation/infection,
- Having poor personal hygiene,
- Having many sexual partners,
- Using tobacco products,
- Human papillomavirus (HPV) infection or HIV may increase the risk of developing penile cancer, and
- UV-A light (i.e. psoriasis treatment)
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean you will not.
Symptoms of Penile Cancer
Symptoms of penile cancer may include
- A sore or lesion on the penis that doesn't heal
- Thickening or a lump on the penis
- Change in colour of the penis
- Itching or bleeding on the penis
- Pain or discomfort during urination
- Discharge from the penis
Metastatic Penile Cancer
Cancer may spread from where it began to other parts of the body. When cancer spreads to another body part, it is called metastasis.
Cancer cells break away from where they began (the primary tumour) and travel through the lymph system or blood.
- Lymph system. Cancer gets into the lymph system, travels through the lymph vessels, and forms a tumour (metastatic) in another body part.
- Blood. Cancer gets into the blood, travels through the blood vessels, and forms a tumour (metastatic) in another body part.
The metastatic tumour is the same type of cancer as the primary tumour. For example, if penile cancer spreads to the lung, the cancer cells in the lung are penile. The disease is metastatic penile cancer, not lung cancer.
Diagnosis of Penile Cancer
Penile cancer is usually diagnosed through a combination of physical examination, imaging tests, and biopsy. The diagnostic process may include
- Physical examination: A doctor will inspect the penis and surrounding area, looking for any lumps or changes in the skin.
- Biopsy: A biopsy is a procedure in which a small tissue sample is removed from the penis and examined under a microscope. This test can confirm the presence of cancer cells and help determine the type of penile cancer.
- Imaging tests: Imaging tests such as computed tomography (CT) scan, magnetic resonance imaging (MRI), or ultrasound may be used to determine the extent of cancer and if it has spread to other parts of the body.
- Additional tests: Additional tests may be needed to determine the cancer stage, such as a CT scan, MRI or a lymphangiography (a special x-ray of the lymph vessels).
Penile cancer can be challenging to diagnose, especially in the early stages. If you have any symptoms or concerns, you should see a doctor as soon as possible.
Penile Cancer Treatment
There are four standard treatments for patients with penile cancer.
- Surgery
- Radiation therapy
- Chemotherapy
- Topical (Biologic) therapy
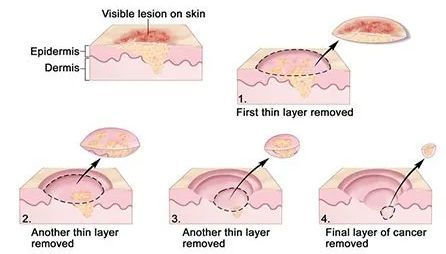
Mohs Microsurgery
A surgical procedure to remove a visible lesion on the skin in several steps.
- First, a thin layer of cancerous tissue is removed.
- Then, a second thin layer of tissue is removed and viewed under a microscope to check for cancer cells.
- More layers are removed one at a time until the tissue viewed under a microscope shows no remaining cancer.
Other Surgical Options
Other surgical options include
- Laser surgery: A surgical procedure that uses a laser beam (a narrow beam of intense light) as a knife to make bloodless cuts in tissue or to remove a surface lesion such as a tumour) with Carbon dioxide (CO2) or neodymium:yttrium-aluminium-garnet (ND: YAG)
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
- Circumcision: Surgery to remove part or all of the foreskin of the penis.
- Wide Local Excision: Surgery to remove only cancer and some normal tissue around it.
- Glans resurfacing or Glansectomy
- Partial or Total Penectomy (Amputation of the penis): Surgery to remove part or all of the penis. If part of the penis is removed, it is a partial penectomy. If all of the penis is removed, it is a total penectomy.
- Inguinal Lymph Node dissection: If penile cancer shows adverse pathological risk factors, including high stage (T2 or higher), high grade or lymphovascular invasion or palpable inguinal lymph nodes.
- Sentinel lymph node biopsy: This surgical procedure is used to determine if cancer cells have spread to the lymph nodes in the groyne. It is less invasive than a complete lymph node dissection (removal of all the lymph nodes in the groyne).
Even if the doctor removes all cancer that can be seen during the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that might be left. Treatment given after the surgery to lower the risk that cancer will come back is called adjuvant therapy.
Radiation Therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
There are two types of radiation therapy.
- External radiation therapy uses a machine outside the body to send radiation toward cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or
- Brachytherapy places a radioactive source directly into or next to penile cancer. A soft urethral tube, called a Foley catheter, is put through the penis and into the bladder to drain urine while brachytherapy is done.
How the radiation therapy is given depends on the type and stage of the cancer being treated.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or preventing them from dividing.
When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
When chemotherapy is placed directly onto the skin (topical chemotherapy) or into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
The way the chemotherapy is given depends on the type and stage of the cancer being treated. Topical chemotherapy (5-FU) may treat stage 0 penile cancer.
Biologic/Immuno-modulating Therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or in a laboratory are used to boost, direct, or restore the body’s natural defences against cancer.
This type of cancer treatment is also called biotherapy or immunotherapy. Topical biologic therapy with Imiquimod may be used to treat stage 0 penile cancer.
What if Penile Cancer is Untreated?
If penile cancer is not treated, it can cause serious health complications, affect the quality of life, and cause severe psychological distress. Symptoms of advanced penile cancer may include pain, difficulty urinating, and changes in the appearance of the penis. In some cases, untreated penile cancer can lead to the removal of the penis or even death.
Seek prompt medical attention if you suspect you may have penile cancer, even if the symptoms are mild or not present. Early detection and treatment of penile cancer can significantly improve the chances of recovery.
Penile cancer can recur, even after treatment, especially in advanced stages. Regular follow-up examinations and imaging tests are essential to detect any recurrence as soon as possible.